Category: Denial Strategies
Strategic Considerations in Revenue Cycle Outsourcing – Onshore,
RCM Vendor Performance: A Guide for Healthcare Providers
In today’s dynamic healthcare landscape, a robust central
Optimizing Collaboration Between Central Billing Offices and Outsourced
Improving Revenue Cycle Management Reporting in Healthcare In
In the dynamic landscape of home health care,
In the realm of home health and hospice
Home health and hospice providers have it tough:
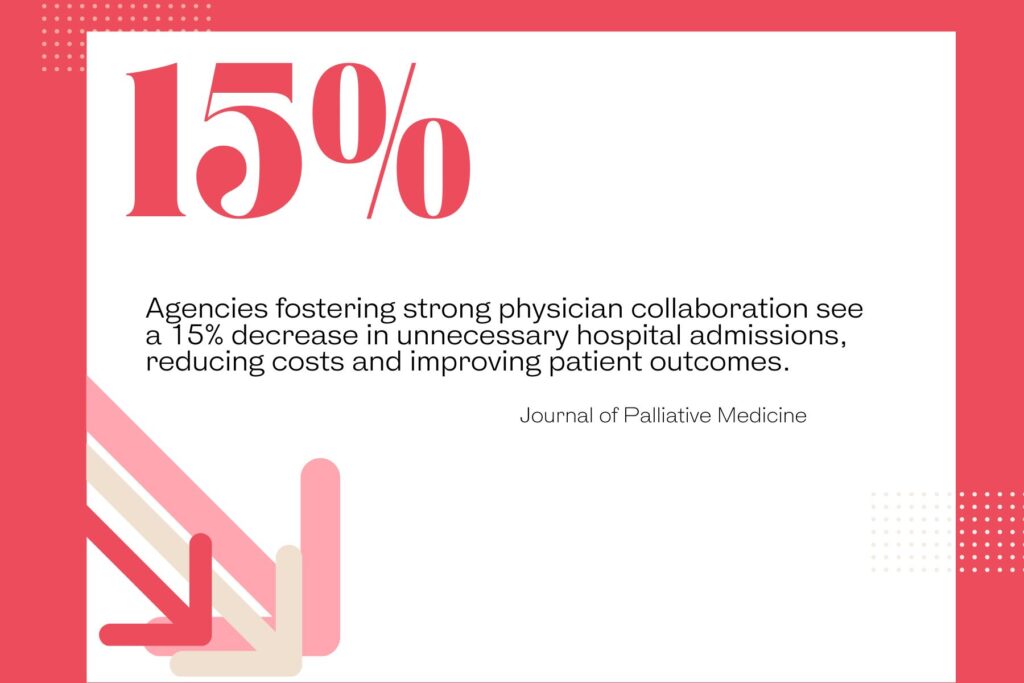
In the realm of hospice care, ensuring a
Ensuring Compliance with Face-to-Face Requirements in Home Health
Improving Fall and Injury Reporting in Home Health
In the dynamic landscape of home health and
Revolutionizing Family Health: A New Approach to Care
The Economics of End-of-Life Care: Understanding Healthcare Spending
Exploring the Challenges of Healthcare Access and Insurance
In the realm of modern healthcare, patient portals
Introduction The healthcare landscape is undergoing a profound
Introduction In today’s rapidly evolving healthcare landscape, the
The Critical Role of Visit Notes in EHR
In today’s rapidly evolving healthcare landscape, the Revenue
The EHR Dilemma: Modernizing Healthcare’s Backbone In our
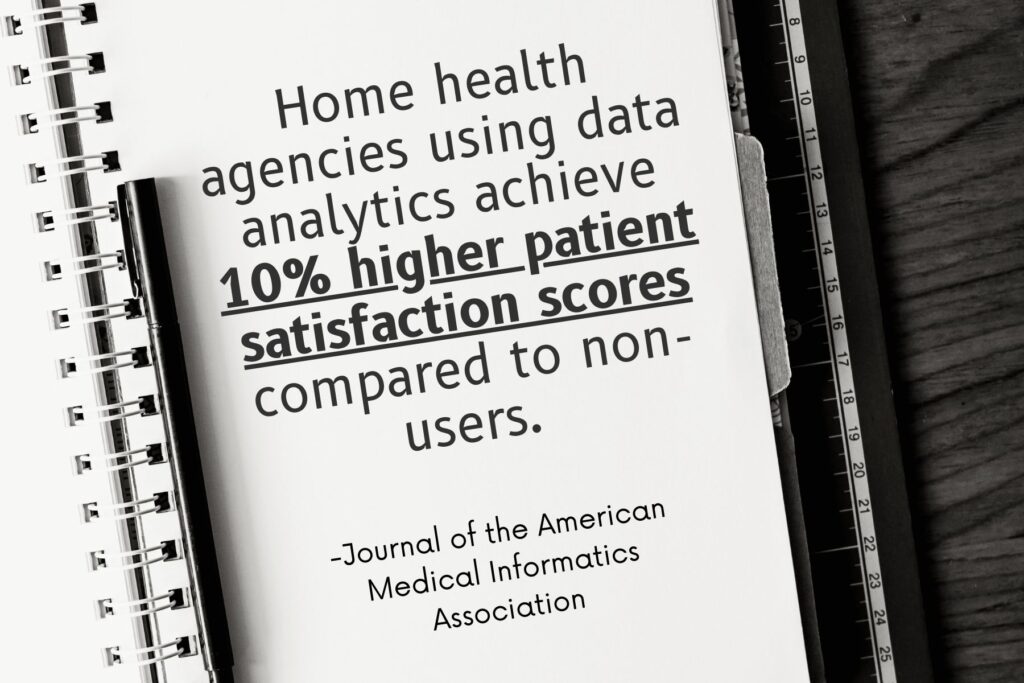
Revolutionizing Healthcare: Advanced Databases Reshape Clinical Care and
Healthcare in the United States is at a
Revolutionizing Healthcare: The Power of AI-Enabled Electronic Health
Introduction Electronic Health Record (EHR) systems revolutionize the
In the intricate landscape of healthcare, Revenue Cycle