Accountability in Revenue Cycle Management Through Analysis and Action
Revenue cycle management (RCM) is a complex and pivotal aspect of healthcare administration, deeply impacted by intricate insurance policies and regulatory requirements. Effective management of this process is crucial for sustaining financial health and operational efficiency.
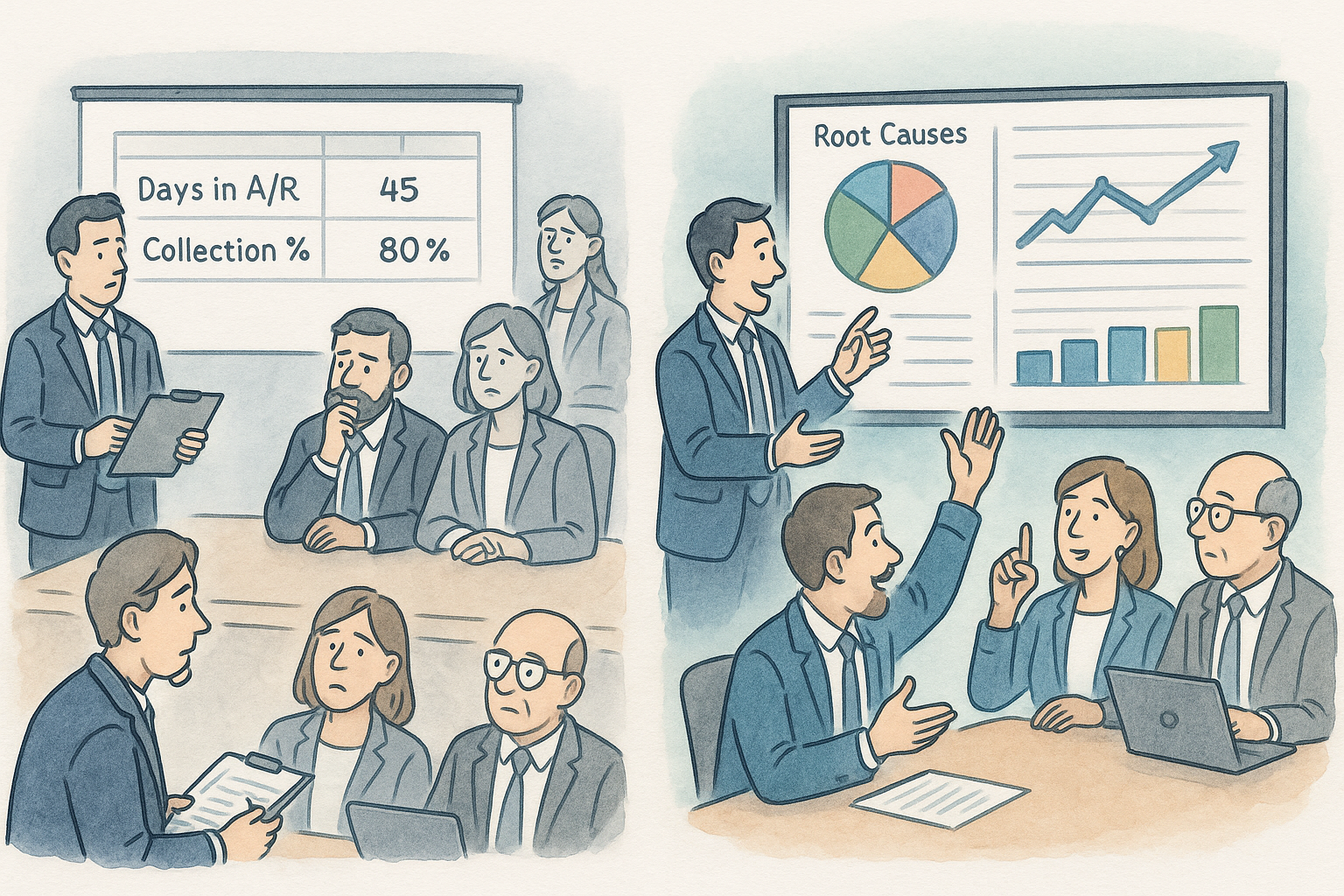
Detailed Review of Adjustments and Denials
One significant challenge in RCM is managing adjustments and understanding the underlying causes of denials. It is essential for revenue cycle directors to actively engage with their data to discern patterns and root causes of recurring issues. For instance, if denials for lack of prior authorization are frequent, this might indicate a systematic oversight rather than isolated incidents. Recognizing such patterns allows for targeted corrective action, ensuring that similar errors are minimized in the future.
Importance of Inquisitive Oversight
A proactive approach involves questioning every aspect of the revenue cycle, from the initiation of patient accounts to the final stages of claims adjustment. Consider a scenario where a large percentage of write-offs are due to non-authorization of services. This situation necessitates a thorough investigation into each case to determine why these denials are not being preemptively addressed. Are the denials concentrated around specific services or tied to particular providers? Such questions can uncover inefficiencies or training gaps in the handling of pre-authorization processes.
Utilizing Data to Drive Improvement
Revenue cycle leaders must ensure that they are not merely passive recipients of reports and data but active participants in the analytical process. It’s not uncommon to find discrepancies in how adjustments are categorized or in the accuracy of payment postings. For instance, a detailed audit might reveal that contractual adjustments are erroneously inflated, masking underpayments or other issues that could impact financial performance.
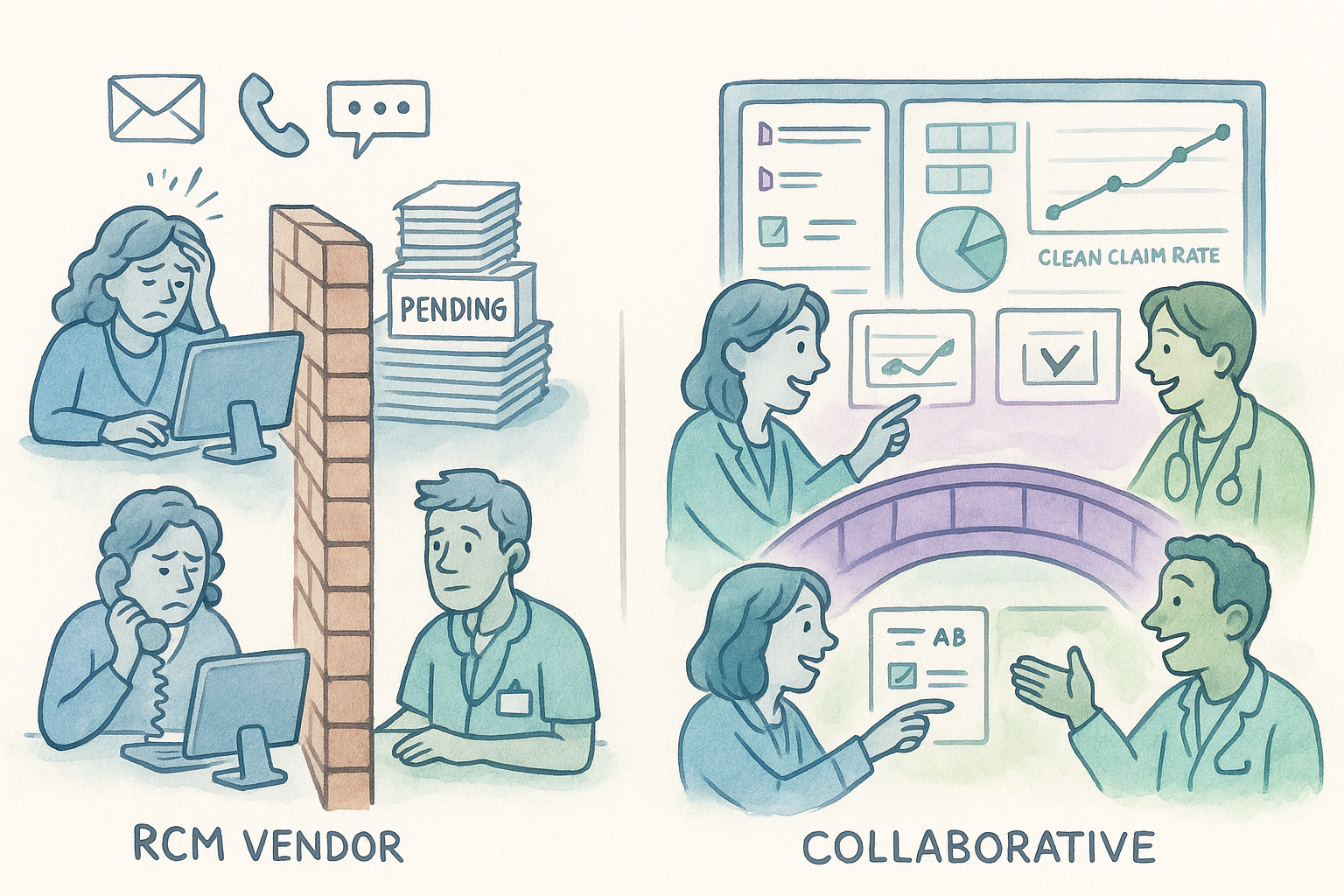
The Role of RCM Vendors in Enhancing Transparency
Communication with RCM vendors is crucial. They should not only provide regular and comprehensive reports but also be responsive to queries and concerns that may arise from their data. For example, if the Medicaid financial class of patients are getting statements, finger-pointing may be to the RCM agency because they handle the claims but they may not be the gatekeeper for patient statements. The perfect case where a candid conversation needs to take place.
Fostering a Culture of Attention to Detail
Ultimately, the effectiveness of a revenue cycle operation hinges on the meticulousness of its management and the quality of the questions its leaders are willing to ask. By fostering a culture of accountability and insisting on detailed, actionable data, healthcare providers can significantly enhance their operational insights and financial outcomes. This proactive stance empowers RCM leaders to anticipate challenges and strategically address them before they escalate into more significant issues, thereby optimizing the financial health of the organization.